Managing Diabetic Eye Disease: Early Signs, Testing, and Treatment Options
Living with diabetes means keeping an eye on more than blood sugar. Over time, diabetes can affect the tiny blood vessels in your retina, the light-sensitive tissue at the back of the eye. When that happens, it is called diabetic eye disease, and the most common form is diabetic retinopathy.
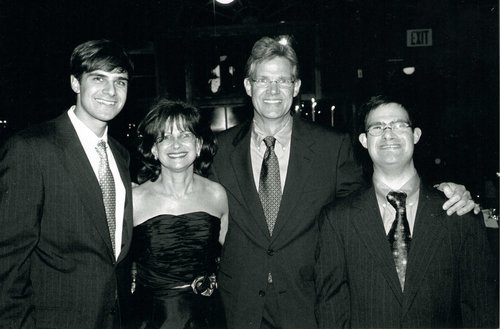
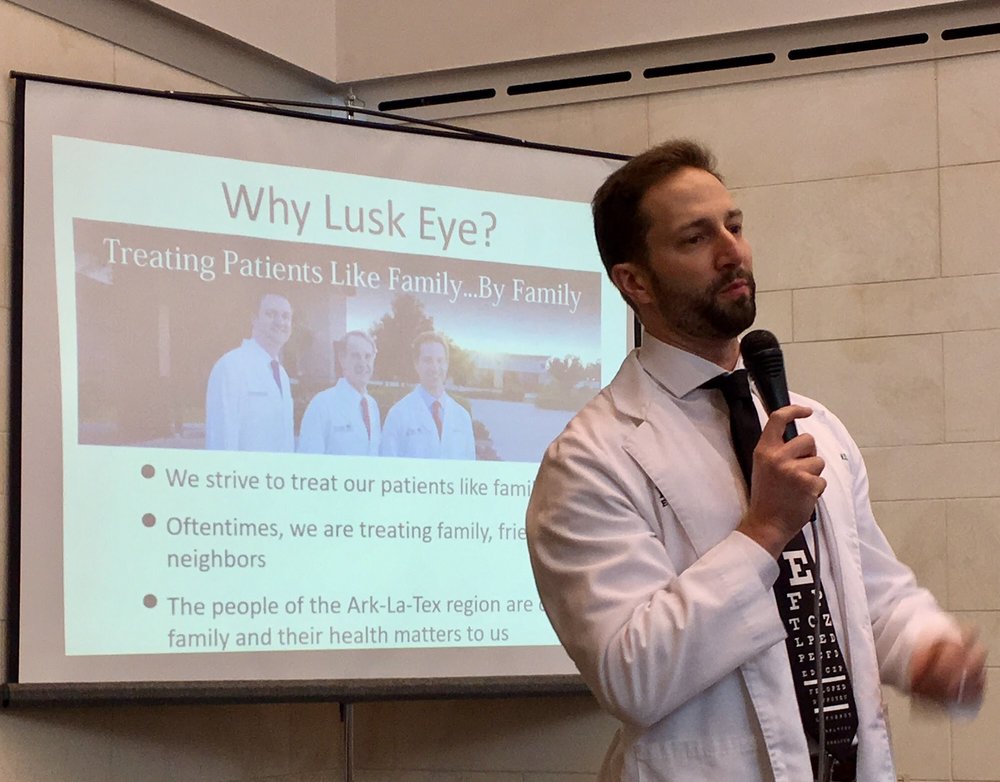
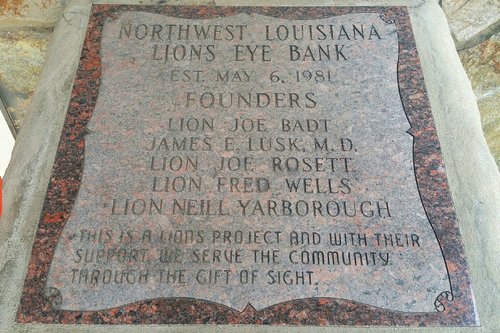
At Lusk Eye Specialists, we see firsthand how powerful early detection can be. Diabetic eye disease often starts quietly, but with the right testing and proper monitoring, serious vision loss is largely preventable. If you have diabetes, here is what you need to know about early warning signs, diabetic retinopathy testing, and today’s retina specialist treatment options.
What is Diabetic Eye Disease?
Diabetic retinopathy happens when prolonged high blood glucose damages retinal blood vessels. These vessels may weaken and leak, or close off, reducing oxygen supply to the retina. In later stages, the eye responds by growing abnormal new vessels that are fragile and prone to bleeding.
Some patients also develop diabetic macular edema (DME), where fluid builds up in the macula—the area responsible for sharp central vision. DME can occur at almost any stage and is a major cause of blurred vision in diabetes.
Early Signs of Diabetic Eye Disease
One of the trickiest things about diabetic retinopathy is that the early stages may not cause noticeable symptoms. That is why the frequency of diabetic eye exams matters so much.
When symptoms do appear, they may include:
- blurred or fluctuating vision
- new floaters or dark spots
- trouble seeing clearly at night
- faded or washed-out colors
- a dark or empty area in your vision
Any sudden change—especially a shower of floaters, flashes, or a “curtain” over your sight—should be treated as urgent. Those can be signs of bleeding or retinal detachment in advanced disease.
Diabetic Retinopathy Testing: How the Disease is Found
Routine testing is the foundation of diabetic eye disease management. At Lusk Eye Specialists, your exam is designed to catch even subtle changes before they threaten vision.
Common tests include:
Comprehensive Dilated Eye Exam
Dilation lets your doctor look directly at the retina and optic nerve to spot microaneurysms, bleeding, swelling, or abnormal vessels.
Retinal Photography/Imaging
High-resolution images document the retina and help track changes over time. This is especially useful for monitoring early or moderate disease.
Optical Coherence Tomography (OCT)
OCT is a quick, non-contact scan that measures retinal thickness and detects macular swelling. It is a key tool for diagnosing and managing DME.
Fluorescein Angiography (when needed)
A specialized dye test that shows blood flow through retinal vessels. It helps confirm areas of leakage or poor circulation and guides treatment planning.
How Often Should You Get a Diabetic Eye Exam?
Guidelines are clear that regular screening is essential, even if your vision feels normal.
General recommendations:
- Type 1 diabetes: first dilated exam within 5 years of diagnosis, then at least yearly.
- Type 2 diabetes: first dilated exam at diagnosis, then at least yearly.
- Pregnancy with diabetes: an exam early in pregnancy, with close follow-up as advised.
If diabetic retinopathy or DME is present, your doctor may recommend exams more often than once a year based on severity and treatment needs.
Specialist Treatment Options
If diabetic eye disease is found, treatment depends on the stage, location, and whether the macula is involved. The goal is always the same: stop progression and protect your sight.
Careful Monitoring
In mild or early cases—especially when changes are in the peripheral retina—monitoring and good systemic control may be all that is needed at first. Lusk Eye Specialists emphasizes close observation in these situations.
Laser Treatment
Laser therapy has long been a mainstay of care and remains a key tool today.
- Focal/grid laser can seal leaking vessels to reduce macular swelling.
- Panretinal photocoagulation (PRP) treats proliferative disease by shrinking abnormal vessels and lowering the risk of severe bleeding.
Lusk Eye Specialists notes that laser therapy may not “cure” retinopathy. Still, it can significantly delay progression and reduce the risk of vision loss.
Injections (anti-VEGF)
Modern care often includes medication injected into the eye to reduce swelling and abnormal vessel growth. Anti-VEGF drugs are a first-line treatment for center-involved DME and can also help control proliferative retinopathy.
These treatments are done in-office and typically given in a series, with the schedule tailored to your response.
Vitrectomy Surgery
For advanced cases with persistent bleeding (vitreous haemorrhage) or traction on the retina, a vitrectomy may be needed. This outpatient surgery removes blood and scar tissue, helping restore sight and prevent retinal detachment.
The Bottom Line
Diabetic eye disease is serious, but it is also highly manageable when caught early. The most critical steps are consistent diabetic retinopathy testing, the right diabetic eye exam frequency, and moving promptly into treatment if changes appear.
Lusk Eye Specialists is here to guide you through every stage—with advanced imaging for early detection, careful monitoring when appropriate, and modern retina specialist treatment options when intervention is needed. If you live with diabetes, protecting your vision starts with one simple habit: keeping your yearly eye exam on the calendar.